What are the Symptoms of Pelvic Floor Dysfunction?
Several symptoms may suggest pelvic floor dysfunction but a complete physical exam should be able to determine what is causing symptoms. Some symptoms of pelvic floor disorder may include:
- Persistent pelvic pain that radiates to the groin, abdomen, and back, and cannot be explained by other causes.
- Constipation or straining pain with bowel movements.
- Leakage of stool/urine with or without awareness.
- Inability to delay urination.
- Inability to tolerate a speculum during a gynecological exam.
- Incomplete emptying of bladder or bowel.
- Ongoing pain in your pelvic region, genitals, or rectum.
- Pain in the back, hips, and sacroiliac joint.
- Pain with wearing tampons.
- Painful intercourse.
- Painful sitting.
- Urinary frequency, burning, or pain.
- Vaginal pain.
Common Causes of Pelvic Floor Dysfunction
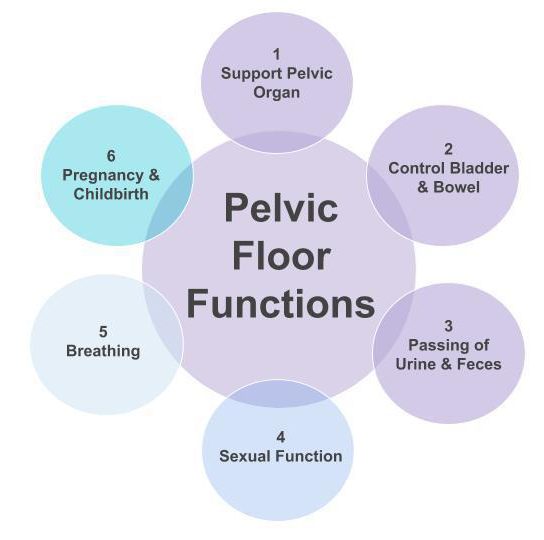
While there are obvious differences between the male and female pelvis the muscles of the pelvic floor are very similar between the two sexes. There are three layers of pelvic floor muscles – superficial and deeper. The role of these muscles includes aiding in sexual function, normal bowel and bladder control, and pelvic organ support.

Prostate surgery: Specific pelvic floor disorders including urinary incontinence and erectile dysfunction are quite common post-operatively. Frequently, after the procedure, these conditions present as having poor bladder control, weakness in pelvic floor muscles (especially urinary sphincters), and changed pelvic nerve supply.

Age: Menopausal age (48-55) increases the risk for developing pelvic organ prolapse and tissue changes.
Endometriosis: Abdominal and pelvic pain, for issues with defecation, urination, constipation, and pain with sex that can all be secondary to endometriosis.
Genetics: Women who have a family history of pelvic organ prolapse and /or weak connective tissue supporting the pelvic floor.
Hysterectomy: Procedure can often damage and weaken the pelvic muscles and is known to increase the chances of developing a pelvic organ prolapse and/or urinary incontinence.
Pregnancy and childbirth: Vaginal birth, prolonged labor, instrumental delivery (use of spoon-like tools to help the baby out of the birth canal) and, episiotomy (a surgical procedure to increase opening in the vagina).

Chronic stress: Being tense can lead to holding breath, tightening muscles and bearing down on pelvic floor.
Constipation: Constipation may be caused by changes in pelvic floor muscles, increase in abdominal pressure during bowel movement and slow transit. These persistent conditions can damage nerves and appear as pelvic floor dysfunction symptoms, such as fecal incontinence.
History of back pain: Lower back pain can be related to pelvic floor muscle dysfunction. This is because the lower back and pelvic floor work closely together. Pain felt in the lower back may travel to the pelvic floor.
Increased abdominal pressure: Frequent coughing (due to chronic lung disease, smoking, allergies) and persistent sneezing causing overuse of pelvic floor muscles.
Intense physical effort: Athletes who engage in high impact sports (e.g. trampolining, running, gymnastics) along with occupations that require frequent heavy lifting add pressure to the bladder and influence urinary incontinence in both genders.
Obesity: Being overweight may be associated with urinary incontinence in both genders and pelvic organ prolapse in women
Pelvic floor injury: Side effects of pelvic radiotherapy can involve changes in and around the pelvic floor muscles in both men and women. In men, radiation for prostate cancer influences erectile dysfunction and urinary incontinence.
Post surgical: Hysterectomy, prolapse repair, hemorrhoidectomy, rectal/bladder cancer, endometriosis, post prostatectomy and back surgery.
Sexual Dysfunction: Menopause can contribute to vulvar tissue changes that can make intercourse difficult. Other conditions may include a history of sexual trauma or abuse and anxiety.